Counseling Suicidal People
Contents:
However, prevention methods cannot be restricted to the individual. Community, social, and policy interventions will also be essential. The act must be deliberately initiated and performed by the person concerned in the full knowledge, or expectation, of its fatal outcome 1. Suicide is among the top 20 leading causes of death globally for all ages and every year, nearly one million people die from suicide.
Worldwide, suicide ranks among the three leading causes of death among those aged 15—44 years, and the second leading cause of death in the 10—24 years age group 2. The global suicide rate is 16 suicides per , inhabitants: Clinical studies have demonstrated that in most countries, suicide predominates in males, although there are important exceptions such as China. Of note, the suicide rate increases with age, although suicide rates among young people have been increasing to such an extent that they are now the group at highest risk in a third of countries, in both developed and developing countries.
As well, there are marked differences in suicide rates between some ethnic groups and individual countries, and also within different regions of one country. A suicide attempt is a self-inflicted, potentially injurious behavior with a nonfatal outcome for which there is evidence either explicit or implicit of intent to die It is estimated that for every suicide, there are 50 suicide attempts, and thus attempts are a source of significant morbidity.
Identifying individuals at imminent risk for suicidal behavior is a major challenge for clinicians. In general, suicide is hard to predict because the prevalence of risk factors is high among the population, while suicide is rare. Indeed, only a minority of those with risk factors will commit suicide. Furthermore, some of the risk factors are not specific and of those who die by suicide, some are not in any risk group.
Despite the challenges in identifying those at risk for suicidal behavior, opportunities for prevention do exist. This contact with the medical profession may afford an opportunity for intervention. More than half of all clinically depressed persons have suicidal ideation and Major Depression Disorder and Bipolar Disorders are the psychiatric disorders most often associated with suicide Some symptoms of depression have been identified as particularly important in risk for suicidal behavior: Effective prevention and treatment of mood disorders might reduce the number of severe suicide attempts, given that most depressed patients at the time of suicide attempt are inadequately treated Thus, treating suicidal depressed patients actively and intensively might offer an effective way of preventing suicidal behavior.
Suicidal ideation is highly prevalent in patients with bipolar disorders, and it is estimated that as many as half of those who have bipolar disorder attempt suicide at least once. The suicide rate among these patients is more than 20 times higher than that of the general population 5 and the risk of suicide is highest early in the course of Bipolar Disorder, particularly in the first year of the illness.
The presence of depressive and dysphoric—irritable states in Bipolar Disorder is reported to be a risk factor for suicide 8. Other work suggests that hopelessness predicts suicidal behavior during the depressive phase, and that severity of depression predicts suicide attempts during mixed episodes Therefore, aggressive and effective management of depressive phases is essential, as depressive phases are high risk periods for suicidal behavior.
Anxiety disorders are associated with lifetime suicidal ideation and suicide attempts, especially in adolescents and in young adults However, whether anxiety disorders alone or whether presence of anxiety in the context of a mood disorder increases risk for suicidal behavior remains an open question. However, Placidi et al 21 found that comorbid panic disorders in patients with major depression did not increase the risk for lifetime suicide attempts. Moreover, non-attempters scored higher in the anxiety items in the Hamilton depression scale.
It may be that anxiety symptoms, like fear of disability or death, serves as a protective factor for suicide. In many PTSD studies, suicidality is associated with comorbid depression and substance abuse Therefore, the increased proportion of suicide attempters among persons with a PTSD diagnosis may be due to the comorbid depression and not to PTSD itself. Given that anxiety is highly comorbid with other mental disorders, especially mood disorders and substance abuse, the role of severe anxiety as a marker of acute suicide risk requires further study.
All substance disorders increase the risk of suicidal behaviors, alcohol being the most significant risk factor among the substances. Alcohol misuse and abuse predispose to impulsivity, aggression, depression, hopelessness, and other negative factors that increase the risk for suicidal behavior. Individuals who commit suicide and suffer from alcohol and other substance abuse disorders are often younger males, divorced or separated. They often suffer from recent adverse life events, and are likely to be intoxicated at the time of the suicide In terms of suicide attempts, the presence of alcohol misuse disorders is also a significant risk factor.
Helping Someone in a Suicidal Crisis
Moreover, when co-morbid with affective disorders, presence of alcohol misuse disorders increases risk of suicide attempts by more than two fold The risk factors for suicide in schizophrenia are past and present suicidal behavior, past depressive episodes, drug abuse or dependence and more frequent psychiatric admissions Of note, other risk factors, such as fear of mental disintegration, agitation or restlessness, and poor adherence to treatment, all increase risk for suicidal behavior and may be more specific to schizophrenia The great majority of suicides in schizophrenia occur in the active phase of the disorder, in the context of depressive symptoms That suicides are most common early in the course of the illness, suggests that prevention and treatment should focus on the early stages of disease.
Personality disorders have been shown to be related to suicidal and self-injurious behavior, both among the general and the psychiatric population Moreover, many suicide attempters meet criteria for a personality disorder 30 , Although borderline personality disorder is the only personality disorder that lists suicidal behavior as a criterion, other personality disorders, such as antisocial and other Cluster B personality disorders 32 also increase risk of suicidal behavior.
Personality disorders are often accompanied by impulsivity, aggression, alcohol and substance abuse, as well as major depressive episodes, all of which are known risk factors for suicide in their own right. Levels of impulsivity, hostility and aggression are higher in suicide attempters compared to non-attempters among people who suffer from major depression Among bipolar patients, past suicide attempters report more lifetime aggression than non-attempters Aggression is an important variable in the prediction of suicidal behavior as well In support of this, older suicides are reported to have lower levels of impulsivity and aggression compared to young suicides.
Hopelessness was found to be associated with future suicide attempts both in the short and long term 19 , 36 , 37 , Furthermore, in mood disorders, it predicts suicidal behavior as part of a pessimism factor, which also includes measures of subjective depression, suicidal ideation and reasons for living [37]. Whether hopelessness as a trait rather than a symptom of depression is of import remains an open question.
Suicidal behavior is highly familial 39 , 3 , 40 and a family history of suicidal behavior is associated with suicide attempts and suicide all through the life cycle and across psychiatric diagnoses This transmission is independent of the transmission of psychiatric disorders 42 , Instead, the familiality of suicidal behavior appears to be mediated by the transmission of a tendency to impulsive aggression, traits that leads the patient to a higher tendency to act upon suicidal thoughts 44 , Childhood trauma is also a risk factor for suicide attempt.
Moreover, the amount of trauma experienced by the child, correlates with younger age at the first suicide attempt and an increased number of suicide attempts [46]. A suicide attempt in the past is a major risk factor for suicide 3 , 16 as well as future suicide attempt, especially among people suffering from affective disorders 46 , 47 , 48 , 49 , 50 , 51 , Repeated suicide attempts increase the risk of future suicidal behavior, as was demonstrated by Leon et al The evidence for suicidal ideation by itself as a risk factor for suicide acts is more nuanced.
In a prospective study [37], suicidal ideation alone did not predict future suicide attempts or completion. In contrast, other studies have identified suicidal ideation as a precursor of attempted and completed suicide among patients with mood disorders 55 , 56 , 57 , 58 and as correlated with greater risk of future suicide attempts as part of a pessimism factor among bipolar patients presenting with a major depressive episode Not surprisingly, suicide attempters also are more likely to endorse suicidal ideation during subsequent acute phases or hospitalizations 60 , 34 Therefore, it is reasonable to view suicide ideation as a risk factor for suicide, either as an independent risk factor, or as part of a complex involving measures of subjective depression, reasons for living, and hopelessness Since a variety of factors are involved in the suicidal act, multimodal approaches covering multiple levels of intervention and activities will be essential to any preventive strategy.
Thus far, prevention strategies found to be effective in suicide prevention include means restriction, responsible media coverage and general public education, as well identification methods such as screening, gatekeeper training, and primary care physician education. Suicide attempts using highly lethal means, such as firearms in US men, or pesticides in rural China, India, and Sri Lanka, result in high rates of death The most frequent means of suicide in Europe is hanging 61 and in North America, firearms Suicide methods are necessarily influenced by their accessibility.
In many countries, restriction of access to common means of suicide has led to lower overall suicide rates For example, increasing firearm control in the US and Canada 64 , 65 , 66 , detoxification of domestic and motor vehicle gas 67 , 68 , restrictions on use of toxic pesticides in rural areas 10 , and physical barriers at jumping sites 69 , 70 are reported to be of utility in reducing suicides. In addition, reducing access to ligature and ligature points in prisons and hospitals has reduced instances of hanging 71 while introducing safer antidepressant, selling smaller packages of analgesics or individually wrapped analgesics, and restricting of the sale of barbiturates has reduced suicides by overdose Thus, public policy to reduce access to means for suicide has an important role in prevention.
Responsible media coverage is key to suicide prevention by providing the public information on mental disorders and their treatment, and ways of identifying persons at risk.
The suicidal person might also be urged to speak with suicide counselors during this time as well. All expressions of suicidality indicate significant distress and heightened vulnerability that require further questioning and action. Summary Positive, empathic attitudes toward clients experiencing suicidal thoughts and behaviors do not, by themselves, mean that clients will initiate or receive appropriate services. Interestingly, the fatality risk of lithium overdoses is moderate, much like that of modern antidepressants and second-generation antipsychotics Signs While not all signs of being suicidal mean that the person will commit the act, you should be able to recognize potential warnings.
Programs to educate the media about coverage of suicides are available through foundations American Foundation for Suicide Prevention and emphasize the importance of reporting suicide as a public health issue, in a non-sensational way. Media coverage should emphasize the treatable causes of suicide, such as substance abuse and mental disorders.
Discussing the available treatment options for these problems and the types of healthcare providers who can treat them may encourage help seeking behavior by those contemplating suicide. As well, because many individuals considering suicide exhibit warning signs, educating the public about such signs can help relatives identify and respond quickly and efficiently to the person in need. In addition, it is essential that media coverage not link suicide only to external events, like divorce, a recent job loss or school failure, dramatic as they may be.
Instead, emphasizing the frequency of psychiatric conditions among those who die by suicide and providing education about possible interventions can be helpful to communities exposed to highly visible suicides. Of note, media reports covering specific suicide methods were found to increase suicidal behaviors in the community in some studies 73 , Therefore, it is advisable to avoid inclusion of specific details such as the location or method of death in news reports.
Before suicidal behavior can be prevented, those at risk need to be identified. Since not all potential suicide attempters are in close contact with a mental health professional, those around them e.
Customers who viewed this item also viewed
Public education campaigns are aimed mostly at improving suicide risk recognition and help-seeking behavior and reducing the stigma of mental illness Some campaigns address suicidal behavior directly, as was done in the United States Air Force suicide prevention program 76 , while others target depressive disorders 77 , 78 , However, Mann et al 10 found no detectable effects of public awareness campaigns, neither on reducing the rate of suicidal acts, or on increasing treatment seeking or antidepressant use. Unfortunately, no study clearly demonstrates increased care seeking or decreased suicidal behavior after such campaigns.
- Find yourself, Build Your Business.
- The Kingdom That Cannot be Shaken.
- How To Become a Suicide Counselor | www.farmersmarketmusic.com;
- Addressing Suicidal Thoughts and Behaviors in Substance Abuse Treatment..
- INTRODUCTION!
- 52 Pickup.
- Petite philosophie de la littérature (French Edition).
However, it still may be the case that awareness campaigns may have an effect when combined with other measures in a multilevel and multifaceted intervention program 81 , This was demonstrated in the Nuremberg Alliance against Depression NAD , a two year intervention program that included four levels: The program demonstrated the additive and synergistic effect of combining all four intervention levels simultaneously. Results of this initiative have yet to be released. However, under-recognition and under-treatment of psychiatric disorders in primary care setting presents a challenge for identifying those at risk and while mental disorders are present in most cases of suicide, most suicides are untreated at the time of death Fortunately, education of primary care physicians in recognition and treatment of depression may be an efficient means for lowering suicide rates 10 , 82 , Indeed, studies that examined programs for primary care physician training found a rise in the antidepressant prescription rates and a decline in the suicide rate after the program 81 , Gatekeepers are figures with the potential to influence the suicidal person on a temporary or ongoing basis e.
The training of gatekeepers focuses on recognizing suicidal thinking and behavior and helping people at risk to access appropriate services The key elements of the training include: Success of gatekeeper training in lowering suicide rates has been reported in military and school programs 84 , In a group-based randomized trial conducted by Wyman et al 85 , QPR Question, Persuade, Refer training of a random sample of school staff increased their knowledge of youth risk factors for suicide.
Screening aims to identify at-risk individuals and direct them to treatment In a study that examined the efficiency of the CSS in identifying high school students at risk of suicide 86 , the algorithm that gave both the highest specificity and the best balance between sensitivity and specificity 0.
A review of studies of depression screening in adults in primary health care settings performed for the US Preventive Services Task Force 87 found higher detection and diagnosis rates of depression through the use of screening tools. It was also found that brief questionnaires, such as the PHQ-2 which ask two questions: Moreover, a review of evidence on screening for suicide risk 88 , suggests that focusing on screening high-risk groups depressed patients, substance abusers in primary care settings may decrease suicide rates.
Since depression is common, affecting about million people worldwide 89 , and the burden of this disease is significant -depression is the 2nd cause of Disability Adjusted Life Years in the age category 15—44 years for both sexes combined and it is expected that by the year , depression will reach that status for all age groups-there may be room to consider depression screening in primary care settings, much like screening for hypertension or diabetes.
Suicide is complex involving psychological, social, biological, cultural and environmental elements.
Therefore, a combination of treatment and support strategies — psychotherapy, pharmacotherapy, follow up treatment and support for those who lost a loved one to suicide, may provide effective measures against suicidal behavior. Several evidence based psychotherapies have been shown to be of utility in the treatment of those at risk for suicidal behavior. This is the case not only because psychotherapy, with or without medication, can reduce depressive symptoms, but because it can specifically target suicidal ideation and suicide attempts For example, Cognitive Behavioral Therapy CBT is an evidence-based method for reducing suicide attempt rates and improving adherence to treatment.
This treatment has been shown to be effective when directly focused on reducing aspects of suicidal behaviour 90 , 91 , 92 , The suicidal person might also be urged to speak with suicide counselors during this time as well.

There is no clear cut method for treating suicidal tendencies in people. During sessions with a suicide counselors, a suicidal person is often gently encouraged to talk about any problems they might be having in their life. Certain types of therapy have also shown to be very promising for individuals contemplating suicide. Cognitive behavioral therapy, for instance, is often used to help people change their negative thoughts. Along with counseling and therapy, a suicide counselor will also usually help a suicidal person come up with a safety plan that can be put into motion when they start to contemplate taking their own lives.
For instance, when a person is feeling suicidal, she can promise to contact her counselor, talk with someone she trusts, go to the hospital, or call a suicide prevention hotline. A suicide counselor can also help a person in despair set up a support network of caring, non-judgmental individuals that she can lean on when times get tough. Because suicide counseling can be such stressful and heartbreaking work sometimes, suicide counselors should also not neglect to tend to their own mental health regularly.
Although they are the counselors, they themselves may sometimes need to seek the help of other mental health professionals in order to cope with things like stress, anxiety, grief, and depression. Suicide counselors might work in a number of different areas. They are often employed by general hospitals, psychiatric hospitals, and mental health clinics. Branches of the military, schools, and social and human service offices also usually have suicide counselors on staff as well.
One of the most well known places for a suicide counselor to work, however, is at a suicide prevention hotline. These positions may be paid or voluntary, and they typically involve answering phones and talking to suicidal individuals. Dealing with suicidal individuals is a very difficult and delicate line of work.
Therefore, the proper education is extremely important when pursuing a suicide counseling career. Some facilities, like suicide prevention hotline facilities, may offer special suicide counseling training to anyone interested in volunteering at the hotline. Colleges and other educational facilities might also offer certificate programs in suicide counseling or suicide prevention. Degree programs in these areas will usually give you a much better and more in depth understanding of suicide as well as the mental and emotional disorders that surround it.
While earning your degree, you should also take several courses that deal with such things as suicide and suicide prevention. The salaries of suicide counselors can vary drastically. Because suicide arouses great fear and anxiety, we actively avoid the topic.
- How To Draw A Rose In Six Easy Steps!
- Can We Really Prevent Suicide?.
- La sonata a Kreutzer (Italian Edition).
- Helping Someone in a Suicidal Crisis // University Counseling Center // University of Notre Dame;
- Je te verrai dans mes rêves (Littérature Française) (French Edition)?
Feelings of guilt and responsibility haunt us. The person in crisis is troubled and has problems that need to be discussed openly.
The number one goal of the therapist should be to help keep the suicidal person alive, so they can then benefit from treatment for their other. What Is Suicide Counseling? Depression is never a pleasant feeling, but some people suffer from depression so severe that they contemplate taking their own.
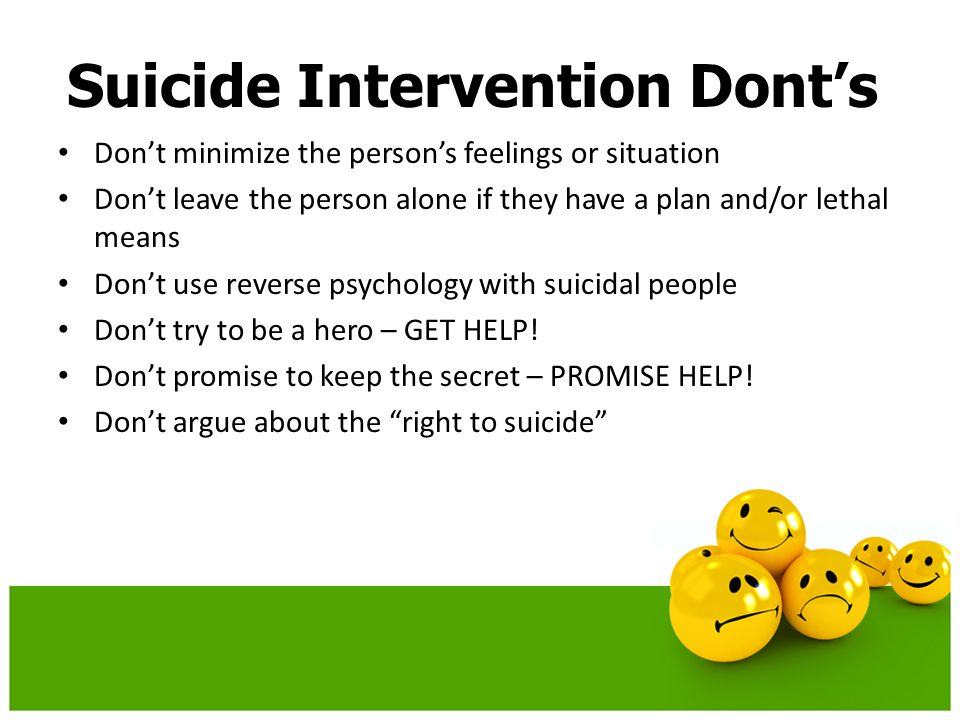
If not taken seriously, the suicidal crisis could worsen. By not asking questions or avoiding the topic, it may seem as if you are not interested. He or she could feel rejected, guilt ridden, and more deeply disturbed. The suicidal person carries a heavy load of guilt and moral arguments only add to this burden.
Suicidal people sometimes make us feel hopeless and impotent, to which we often respond by becoming belligerently helpful. We urge the potential suicide to live in order to justify ourselves. Emotional exhortations based upon our own needs are futile. You may be tempted to try to rescue your friend by telling him or her, for example, that her or she is a good person and that life is worthwhile.
- The Sensuous Casino Dealer
- Das Verhältnis von Staat und Geschlecht aus feministischer Perspektive (German Edition)
- Preactive Leadership
- The Dude and the Zen Master
- Australia: Handsome Heroes: His Secret Love-Child / The Doctors Unexpected Proposal / Pregnant with His Child (Mills & Boon M&B) (Crocodile Creek 24-hour Rescue, Book 1): hour Rescue - 1
- She Aint a Lady