Multistep Cognitive Behavioral Therapy for Eating Disorders: Theory, Practice, and Clinical Cases
Contents:
Received Jun 6; Accepted Jun 6. Book review, Cognitive behavioral theraphy, Eating disorders. Competing interests The author declares that she has no competing interests. Cognitive behaviour therapy for eating disorders: A cognitive behavioral approach to the management of bulimia. Cognitive Behavior Therapy and Eating Disorders. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: A randomized controlled trial of psychoanalytic psychotherapy or cognitive-behavioral therapy for bulimia nervosa.
A randomized controlled comparison of integrative cognitive-affective therapy ICAT and enhanced cognitive-behavioral therapy CBT-E for bulimia nervosa.
Multistep Cognitive Behavioral Therapy for Eating Disorders
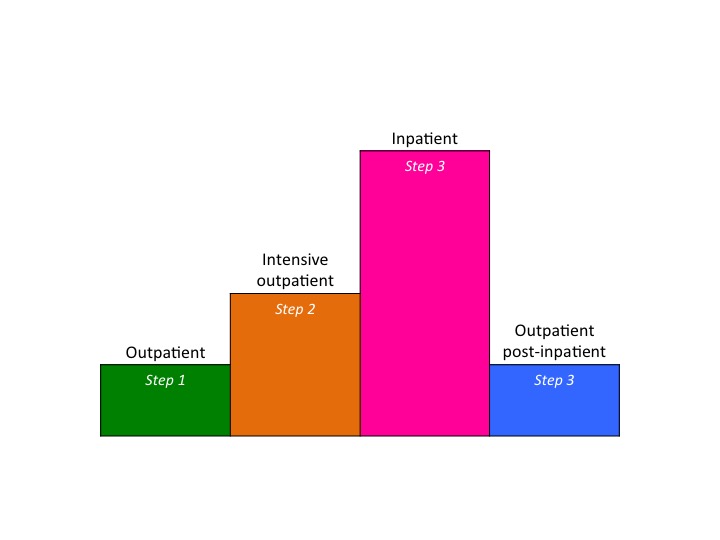
Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatients with anorexia nervosa ANTOP study: The effectiveness of enhanced cognitive behavioural therapy for eating disorders: It is designed to be applicable to three different levels of care outpatient, intensive outpatient, inpatient , and to eating disorder patients of all diagnostic categories, ages, and BMI categories. Distinguishing multistep CBT-E is the adoption of a multi-step approach conducted by a multidisciplinary CBT-E team including psychologists, dietitians, and physicians, the inclusion of a family module for patients under eighteen years old, and the use of assisted eating and group sessions, in adjunct to individual psychotherapy in the intensive levels of care.
The first eight chapters provide an overview of eating disorders, the cognitive behavior theory of eating disorders, how to build a CBT-E multidisciplinary team, how patients are assessed and prepared for the treatment, the general organization, procedures, and strategies involved in the three steps of multistep CBT-E treatment, and how multistep CBT-E can be adapted for adolescents.
In order to highlight the flexibility of the multistep CBT-E approach, Section Two of the book provides a detailed description of three treated clinical cases. The first case illustrates how outpatient CBT-E was adapted to treat a professional sportswoman affected by an eating disorder; the second describes the procedures and strategies applied in intensive outpatient CBT-E to treat a patient who did not improve with standard outpatient CBT-E; and the third case illustrates the procedures and strategies typically applied in inpatient CBT-E and shows how it can be used to help a patient with a longstanding eating disorder who has failed to respond to several outpatient treatments.
Each chapter gives a general description of the case in question and details the main procedures, strategies, and tools used from the assessment stage through to discharge. In addition, abridged transcripts of relevant clinical sessions are included, to give interesting insight into the practical implementation of multistep CBT-E, and the outcomes at the end of the treatment and follow-up are reported.
To help them adopt these complex behaviors, patients are educated that it is necessary for them to develop a long-term weight-control mind-set. They should also be taught to identify and act upon early signs of relapse ie, changes in eating and physical activity habits and to implement a preestablished plan immediately when their body weight goes beyond the weight-maintenance binary of 2 kg. Patients are encouraged to maintain the lifestyle modifications adopted during phase 1, particularly their active lifestyle, regular eating ie, three meals and two snacks a day , and diet.
They are also reminded to follow a flexible eating plan without being influenced by food cravings: At this stage it is also important to emphasize to patients that their attitude to any setback is crucial in determining its consequences. Toward the end of this phase, patients are instructed in self-efficacy.
- Little Book of Britain At War?
- Multistep Cognitive Behavioral Therapy for Eating Disorders : Theory, Practice, and Clinical Cases!
- Book details.
- Peter Gaymanns Wellness-Hühner (German Edition)!
- Der Einfluss von Dividenden auf Aktienrenditen (Empirische Finanzmarktforschung/Empirical Finance) (German Edition)!
They are encouraged to suspend use of their monitoring records, and in their place are helped to build a written weight-maintenance plan. This should include both the behavioral and cognitive procedures designed to maintain their weight, as well as those that will help them deal with any potential setbacks. They are also invited to attend posttreatment review sessions at 20 and 40 weeks after the end of treatment. These sessions are focused on discussing their progress and any obstacles they have met while attempting to maintain weight, and adjusting their weight-maintenance plan as appropriate.
Both diets also produced a similar improvement in cardiovascular risk factors and psychological profiles.
A combination of factors is likely to have influenced these positive outcomes. In particular, the initial residential period undoubtedly promoted adherence to lifestyle changes, as patients were not exposed to additional food stimuli and were led in gradual daily physical activity rehabilitation by a CBT-OB physiotherapist. Long-term adherence after discharge was also likely promoted by the deconditioning of patients from their food- and non-food-related eating stimuli achieved during the 3 weeks of inpatient treatment. In fact, a recent study to compare the long-term effects of residential CBT-OB in 54 patients with severe obesity with or without binge-eating disorder BED 52 found that after 5 years of follow-up, There was no difference in mean weight loss between the two groups of patients 6.
Multistep CBT-OB was developed on the basis of these encouraging results, and is currently being assessed in two ongoing observational outpatient studies one that delivers the treatment individually and one in group sessions conducted in a real-world clinical setting. Multistep CBT-OB is a new treatment that can be delivered at three levels of care outpatient, day hospital, and residential in empirical and logical steps designed to minimize cost and intrusiveness and maximize outcomes. The treatment seeks to address some of the main flaws in BT-OB that could limit its long-term efficacy in treating obesity, ie, the lack of individualization, and the prevalent focus on the behaviors implicated in weight loss and maintenance at the expense of cognitive processes influencing long-term adherence to lifestyle modification.
Moreover, it is suitable for treating patients with severe obesity and associated medical comorbidities and disability, who are generally referred for bariatric surgery rather than attempting less invasive approaches. If the promising findings thus far reported for residential CBT-OB are confirmed in the long term and by ongoing studies on outpatient CBT-OB, multistep CBT-OB has the potential to provide a more efficacious alternative to traditional weight-loss lifestyle modification for patients with obesity.
Lifestyle modification in the management of obesity: Social Foundations of Thought and Action: A Social Cognitive Theory.
Personalized multistep cognitive behavioral therapy for obesity
Cognitive Therapy of Depression: Behavior therapy and cognitive-behavioral therapy of obesity: J Am Diet Assoc. Lifestyle modification for the management of obesity. Interpreting weight losses from lifestyle modification trials: Int J Obes Lond.
J Am Coll Cardiol. Treatment of obesity by very low calorie diet, behavior therapy, and their combination: Environmental influences on eating and physical activity. Annu Rev Public Health. Look Ahead Research Group. Eight-year weight losses with an intensive lifestyle intervention: Behavioral strategies of individuals who have maintained long-term weight losses. A cognitive profile of obesity and its translation into new interventions.
- The Berenstain Bears Discover Gods Creation (Berenstain Bears/Living Lights);
- Resources - Rewrite Your Story!
- Awaken Your Authentic Leadership - Lead with Inner Clarity and Purpose.
- Multistep cognitive behavioural therapy for eating disorders?
- 25 Ways to Sew Jelly Rolls, Layer Cakes & Charm Packs: Modern Quilt Projects from Contemporary Pre-cuts.
The influence of weight-loss expectations on weight loss and of weight-loss satisfaction on weight maintenance in severe obesity. J Acad Nutr Diet. The influence of cognitive factors in the treatment of obesity: Assessing the appropriateness of the level of care for morbidly obese subjects: Rehabilitation in obesity with comorbidities: Cognitive-Behavioral Treatment of Obesity: A randomized controlled trial of two weight-reducing short-term group treatment programs for obesity with an month follow-up.
Int J Behav Med. Adding cognitive therapy to dietetic treatment is associated with less relapse in obesity. Acceptance-based versus standard behavioral treatment for obesity: Testing a new cognitive behavioural treatment for obesity: Weight loss expectations and attrition in treatment-seeking obese women.
Weight loss expectations in obese patients and treatment attrition: Continuous care in the treatment of obesity: The Look Ahead study: Diabetes Prevention Program Research Group.
The Learn Program for Weight Management. Cognitive Behavior Therapy and Eating Disorders. Theory, Practice, and Clinical Cases. Complexity of attrition in the treatment of obesity: Impact of an intensive lifestyle intervention on use and cost of medical services among overweight and obese adults with type 2 diabetes: Weight change in the first 2 months of a lifestyle intervention predicts weight changes 8 years later.
Self-monitoring in weight loss: Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Engl J Med.
4 editions of this work
A biometric study of human basal metabolism. J Nutr Educ Behav. Systematic review of the Mediterranean diet for long-term weight loss. Health benefits of the Mediterranean diet: