Future Directions in Regenerative Medicine
Contents:
To date, regenerative medicine has led to new, FDA-approved therapies being used to treat a number of pathologies. Considerable research has enabled the fabrication of sophisticated grafts that exploit properties of scaffolding materials and cell manipulation technologies for controlling cell behavior and repairing tissue. These scaffolds can be molded to fit the patient's anatomy and be fabricated with substantial control over spatial positioning of cells.
Strategies are being developed to improve graft integration with the host vasculature and nervous system, particularly through controlled release of growth factors and vascular cell seeding, and the body's healing response can be elicited and augmented in a variety of ways, including immune system modulation.
- Le programme de Belleville. Décryptage (Les grands textes politiques décryptés t. 12) (French Edition);
- There was a problem providing the content you requested?
- La casa de mamá (Spanish Edition).
- ;
New cell sources for transplantation that address the limited cell supply that hampered many past efforts are also being developed. A number of issues will be important for the advancement of regenerative medicine as a field. First, stem cells, whether isolated from adult tissue or induced, will often require tight control over their behavior to increase their safety profile and efficacy after transplantation. The creation of microenvironments, often modeled on various stem cell niches that provide specific cues, including morphogens and physical properties, or have the capacity to genetically manipulate target cells, will likely be key to promoting optimal regenerative responses from therapeutic cells.
Second, the creation of large engineered replacement tissues will require technologies that enable fully vascularized grafts to be anastomosed with host vessels at the time of transplant, allowing for graft survival. Thirdly, creating a proregeneration environment within the patient may dramatically improve outcomes of regenerative medicine strategies in general.
- Regenerative medicine: Current therapies and future directions..
- Regenerative nanomedicine: current perspectives and future directions.
- La flauta de ónix (Spanish Edition);
- The Taxpayer - July 2012 (The Taxpayer 2012 Book 61).
- Shadows on the Mountain: The Allies, the Resistance, and the Rivalries that Doomed WWII Yugoslavia.
- Miriams Family Life (Miriams Life Book 4)!
An improved understanding of the immune system's role in regeneration may aid this goal, as would technologies that promote a desirable immune response. A better understanding of how age, disease state, and the microbiome of the patient affect regeneration will likely also be important for advancing the field in many situations — Finally, 3D human tissue culture models of disease may allow testing of regenerative medicine approaches in human biology, as contrasted to the animal models currently used in preclinical studies.
Increased accuracy of disease models may improve the efficacy of regenerative medicine strategies and enhance the translation to the clinic of promising approaches The authors declare no conflict of interest. National Center for Biotechnology Information , U.
Published online Nov Mao a, b and David J. Mooney a, b, 1. Mao a John A. Mooney a John A. Author information Copyright and License information Disclaimer. Edited by Mark E.

This article has been cited by other articles in PMC. Abstract Organ and tissue loss through disease and injury motivate the development of therapies that can regenerate tissues and decrease reliance on transplantations. Therapies in the Market Since tissue engineering and regenerative medicine emerged as an industry about two decades ago, a number of therapies have received Food and Drug Administration FDA clearance or approval and are commercially available Table 1. Regenerative medicine FDA-approved products.
Open in a separate window. Therapies at the Preclinical Stage and in Clinical Testing A broad range of strategies at both the preclinical and clinical stages of investigation are currently being explored. Recapitulating Tissue and Organ Structure. Altering the Host Environment: Cell Infusions and Modulating the Immune System. Existing and New Cell Sources. Conclusion To date, regenerative medicine has led to new, FDA-approved therapies being used to treat a number of pathologies.
Footnotes The authors declare no conflict of interest. Tissue Eng Part B Rev. An FDA perspective on preclinical development of cell-based regenerative medicine products.
Regenerative medicine: Current therapies and future directions
Mendelson A, Frenette PS. Hematopoietic stem cell niche maintenance during homeostasis and regeneration. Regenerative medicine and solid organ transplantation from a historical perspective. Regenerative Medicine Applications in Organ Transplantation. Annu Rev Biomed Eng. Kami D, Gojo S. From insights to vertebrate regeneration. Opportunities in regenerative medicine. Tissue engineering and regenerative medicine: Recent innovations and the transition to translation.
Evolution of autologous chondrocyte repair and comparison to other cartilage repair techniques. Falanga V, Sabolinski M. Huebsch N, Mooney DJ. Inspiration and application in the evolution of biomaterials. A prospective, multicentre, randomised controlled study of human fibroblast-derived dermal substitute Dermagraft in patients with venous leg ulcers. Organ engineering based on decellularized matrix scaffolds.
J Thorac Cardiovasc Surg. Classic options, novel strategies, and future directions.
Papanas N, Maltezos E. Becaplermin gel in the treatment of diabetic neuropathic foot ulcers. Basic science and spine literature document bone morphogenetic protein increases cancer risk. A closer look at bioengineered alternative tissues. Stem cell therapy and regenerative medicine. The price of innovation: New estimates of drug development costs. Methodologic and policy considerations.
N Engl J Med. Kaplan AV, et al. From prototype to regulatory approval. Of extracellular matrix, scaffolds, and signaling: Tissue architecture regulates development, homeostasis, and cancer. Annu Rev Cell Dev Biol. An overview of tissue and whole organ decellularization processes. Macchiarini P, et al. Clinical transplantation of a tissue-engineered airway. Petersen TH, et al. Tissue-engineered lungs for in vivo implantation.
Uygun BE, et al. Organ reengineering through development of a transplantable recellularized liver graft using decellularized liver matrix. Decellularized rhesus monkey kidney as a three-dimensional scaffold for renal tissue engineering. Tissue Eng Part A. Goh SK, et al. Perfusion-decellularized pancreas as a natural 3D scaffold for pancreatic tissue and whole organ engineering. Mase VJ, Jr, et al. Clinical application of an acellular biologic scaffold for surgical repair of a large, traumatic quadriceps femoris muscle defect. Dahl SL, et al.
Readily available tissue-engineered vascular grafts. Fishman JM, et al. Expert Opin Biol Ther. Decellularization and recellularization of three-dimensional matrix scaffolds. The design of scaffolds for use in tissue engineering. Development of biocompatible synthetic extracellular matrices for tissue engineering. Hydrogels for tissue engineering: Scaffold design variables and applications. Wong T, et al. Potential of fibroblast cell therapy for recessive dystrophic epidermolysis bullosa. Patterson JT, et al. Tissue-engineered vascular grafts for use in the treatment of congenital heart disease: From the bench to the clinic and back again.
Roh JD, et al. Tissue-engineered vascular grafts transform into mature blood vessels via an inflammation-mediated process of vascular remodeling. Hibino N, et al. Tissue-engineered vascular grafts form neovessels that arise from regeneration of the adjacent blood vessel. Application of tissue engineering to the immune system: Development of artificial lymph nodes. Dual growth factor delivery and controlled scaffold degradation enhance in vivo bone formation by transplanted bone marrow stromal cells. Growth factor delivery-based tissue engineering: General approaches and a review of recent developments.
J R Soc Interface. Tissue-engineered autologous bladders for patients needing cystoplasty. Kolambkar YM, et al. An alginate-based hybrid system for growth factor delivery in the functional repair of large bone defects. Ballyns JJ, et al. Image-guided tissue engineering of anatomically shaped implants via MRI and micro-CT using injection molding. Imaging challenges in biomaterials and tissue engineering.
Tissue Eng Part B Rev. Regenerative medicine, an interdisciplinary field that applies engineering and life science principles to promote regeneration, can potentially restore diseased and injured tissues and whole organs. Increased accuracy of disease models may improve the efficacy of regenerative medicine strategies and enhance the translation to the clinic of promising approaches Microextrusion bioprinting dispenses a continuous stream of ink onto a stage In some cases, the polymer's mechanical properties alone are believed to produce a therapeutic effect. This review will first discuss regenerative medicine therapies that have reached the market.
Ajalloueian F, et al. Biomechanical and biocompatibility characteristics of electrospun polymeric tracheal scaffolds. Guven S, et al. Multiscale assembly for tissue engineering and regenerative medicine. Untethered micro-robotic coding of three-dimensional material composition. Bioprinting scale-up tissue and organ constructs for transplantation. Murphy SV, Atala A. Inkjet printing as a deposition and patterning tool for polymers and inorganic particles.
Thermal inkjet printing in tissue engineering and regenerative medicine. Recent Pat Drug Deliv Formul. Printing and prototyping of tissues and scaffolds. Xu T, et al. Hybrid printing of mechanically and biologically improved constructs for cartilage tissue engineering applications. J Biomed Mater Res A. Kolesky DB, et al. A novel recovery system for cultured cells using plasma-treated polystyrene dishes grafted with poly N-isopropylacrylamide J Biomed Mater Res.
Nakajima K, et al. Intact microglia are cultured and non-invasively harvested without pathological activation using a novel cultured cell recovery method. Yamato M, Okano T. Nishida K, et al. Corneal reconstruction with tissue-engineered cell sheets composed of autologous oral mucosal epithelium. Scaffold-free vascular tissue engineering using bioprinting. Organogenesis from stem cells in 3D culture.
Sato T, et al. Paneth cells constitute the niche for Lgr5 stem cells in intestinal crypts. Vascularization strategies for tissue engineering. Battler A, et al. Intracoronary injection of basic fibroblast growth factor enhances angiogenesis in infarcted swine myocardium. J Am Coll Cardiol. Vascular development comes of age. Molecular mechanisms of blood vessel growth. Spatiotemporal control of vascular endothelial growth factor delivery from injectable hydrogels enhances angiogenesis.
The effect of the controlled release of basic fibroblast growth factor from ionic gelatin-based hydrogels on angiogenesis in a murine critical limb ischemia model. Polymeric system for dual growth factor delivery. Mimicking nature by codelivery of stimulant and inhibitor to create temporally stable and spatially restricted angiogenic zones. Engineering and characterization of functional human microvessels in immunodeficient mice.
Therapies in the Market
Chen X, et al. Prevascularization of a fibrin-based tissue construct accelerates the formation of functional anastomosis with host vasculature. The role of endothelial progenitor cells in prevascularized bone tissue engineering: Development of heterogeneous constructs. Formation of human capillaries in vitro: The engineering of prevascularized matrices.
Lesman A, et al. Engineering vessel-like networks within multicellular fibrin-based constructs. Mikos AG, et al. Prevascularization of porous biodegradable polymers. Levenberg S, et al. Engineering vascularized skeletal muscle tissue. Dvir T, et al. Prevascularization of cardiac patch on the omentum improves its therapeutic outcome. Warnke PH, et al. Growth and transplantation of a custom vascularised bone graft in a man.
Finally, we propose directions for current and future regenerative medicine therapies. Keywords: regenerative medicine, tissue engineering. Proc Natl Acad Sci U S A. Nov 24;(47) doi: /pnas. Regenerative medicine: Current therapies and future directions.
Zhang B, et al. A biodegradable scaffold with built-in vasculature for cardiac tissue vascularization and surgical vascular anastomosis.
Post your comment
Hasan A, et al. Microfluidic techniques for development of 3D vascularized tissue. Pepper AR, et al. A prevascularized subcutaneous device-less site for islet and cellular transplantation. Anand P, et al. The role of endogenous nerve growth factor in human diabetic neuropathy. Tuszynski MH, Steward O. Concepts and methods for the study of axonal regeneration in the CNS. Griffith M, et al. A regenerative medicine approach.
Eye Lond ; 23 Biomaterial-based delivery for skeletal muscle repair. Adv Drug Deliv Rev. Suuronen EJ, et al. Functional innervation in tissue engineered models for in vitro study and testing purposes. Growth factor enhancement of peripheral nerve regeneration through a novel synthetic hydrogel tube. Matrix inclusion within synthetic hydrogel guidance channels improves specific supraspinal and local axonal regeneration after complete spinal cord transection. Angiogenesis in life, disease and medicine. Borselli C, et al. Functional muscle regeneration with combined delivery of angiogenesis and myogenesis factors.
Shvartsman D, et al. Forbes SJ, Rosenthal N. Preparing the ground for tissue regeneration: From mechanism to therapy. Taguchi A, et al. Bird TG, et al. Bone marrow injection stimulates hepatic ductular reactions in the absence of injury via macrophage-mediated TWEAK signaling.
Alteration of skin properties with autologous dermal fibroblasts. Int J Mol Sci. Environmentally responsive therapeutics for regenerative medicine. Lee RH, et al. Intravenous hMSCs improve myocardial infarction in mice because cells embolized in lung are activated to secrete the anti-inflammatory protein TSG Krampera M, et al. Role for interferon-gamma in the immunomodulatory activity of human bone marrow mesenchymal stem cells. Delivery routes and engraftment, cell-targeting strategies, and immune modulation.
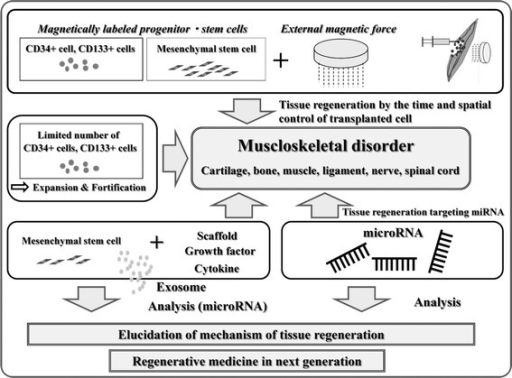
Tomei AA, et al. Device design and materials optimization of conformal coating for islets of Langerhans. Targeted delivery of progenitor cells for cartilage repair. Cheng Z, et al. Unfortunately classic options such as auto- and allografts have significant limitations and thus, alternative strategies should be used to reconstruct such large bone defects [1]. Another goal is to accelerate and enhance the quality of the bone repair in the shortest possible time [ 1 ]. In the last decade, tissue engineering and regenerative medicine TERM in its new concept by means of combination of tissue scaffolds, healing promotive factors and cells or stem cells have been introduced to orthopedic research and sports medicine [ 1 , 2 ].
Although several TERM based products have been introduced to the market in the recent years, none of them provided an acceptable solution with favorable outcome at long term follow-up [ 2 ]. Novel strategies using TERM based products are still under investigation. For designing a suitable bone substitute TERM based graft, some important characteristics have to be considered including, osteoconduction, osteoinduction, osteoincorporation, osteointegration and osteogenesis [ 2 ]. In addition, the graft should have biocompatibility and biodegradability [ 2 ].
To date, no TERM based graft having all the above mentioned characteristics has been designed, manufactured and its efficacy on bone healing and regeneration investigated. To design such a desirable graft, two points should be kept in mind including: To address these issues, the graft should be produced by using natural based polymers such as collagen, elastin, gelatin, hydroxyapatite, chitosan and three- or octa calcium phosphate [ 2 ]. These polymers provide optimum grades of biocompatibility and biodegradability. Unfortunately, most of the commercially available grafts are produced from synthetic polymers such as polyglycolic acid, polygalactin , and polydioxanone having low biodegradability and prolong the chronic inflammation which is not clinically pleasant [ 2 ].
Natural polymers have also an optimum osteoconductivity; the ability of a graft to guide tissue regeneration between bone edges [ 2 ]. However the biodegradability of the natural polymers is fast thus the implanted graft may not contributed in all parts of the healing process therefore, combining natural rapid absorbable as major part with synthetic low absorbable as minor part polymers, a hybrid scaffold can be produced with controllable absorbability [ 2 , 3 ].
Using natural polymers as major part of a graft also increases the osteoincorporative and osteointegrative properties of a TERM based graft because natural molecules have excellent bioactivity during bone repair [ 2 ]. The major challenge is the osteoinductivity of the TERM based grafts. In fact, there are few options for inducing bone mineralization and bone formation so that most of the TERM based grafts can only trigger osteoconduction with low effectiveness on osteoinduction.
In such cases, the new tissue fills the defect completely but has inferior mechanical property so that it would not be able to tolerate weight bearing forces due to the lack of mineralization [ 2 , 3 ]. The most investigated osteoinductive agent is a group of bone morphogenetic proteins BMPs , in which the type II is a popular type [ 3 ]. However, the BMPs have significant limitations and their high cost is their most important limitation [ 3 ].
Alternative osteoinductive agents are currently under investigation [ 4 - 8 ]. Platelet rich plasma and platelet gel are natural sources of growth factors and could contribute to bone induction however concerns are arising in their real efficacy on the healing process [ 2 , 4 ]. Recent studies have suggested that platelets may have only a modulatory role on inflammation and their growth factors may not be a major contributor during healing [ 4 ].